Hydroxychloroquine: Ophthalmological Monitoring and Key Adverse Effects in Autoimmune Diseases
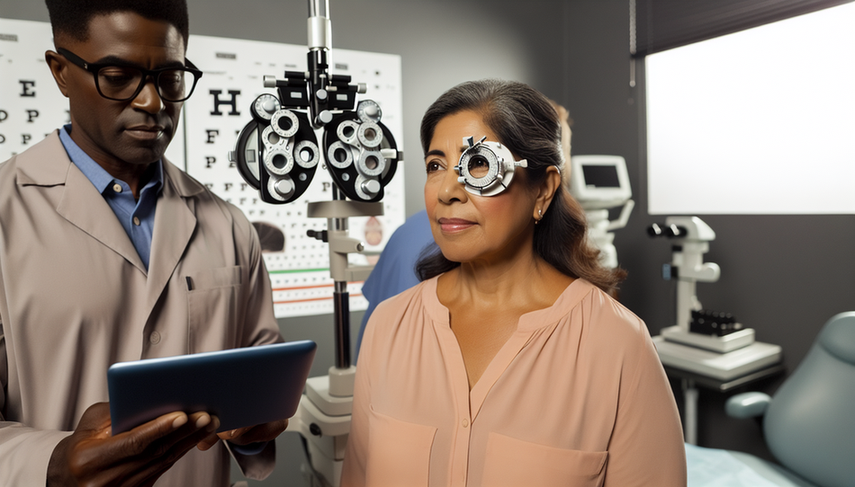
Hydroxychloroquine is a widely used medication in the treatment of autoimmune diseases such as systemic lupus erythematosus and rheumatoid arthritis. While its therapeutic benefits are well recognized, prolonged use can lead to significant adverse effects, with retinopathy being one of the most concerning. Blurred vision and other visual problems may indicate retinal toxicity, highlighting the importance of regular ophthalmological control in patients receiving this treatment.
Ophthalmological Monitoring and Hydroxychloroquine-Induced Retinopathy
Hydroxychloroquine-induced retinopathy is a serious complication that can result in irreversible vision loss if not detected in time. Ophthalmological monitoring is crucial for identifying pre-symptomatic changes and preserving visual function. Current guidelines recommend performing visual field tests and optical coherence tomography (OCT) after five years of continuous use of the medication.
A recent study in the United Kingdom highlighted that the coverage of monitoring is low, resulting in a high percentage of symptomatic diagnoses. Furthermore, adherence to the American Academy of Ophthalmology guidelines has been found to be poor, particularly regarding the initiation and frequency of control examinations, which can lead to late diagnoses of retinopathy [1].
Other Relevant Adverse Effects
In addition to retinopathy, hydroxychloroquine can cause other significant adverse effects. These include induced cardiomyopathy and skin hyperpigmentation. Although less common, cardiomyopathy is a serious complication that requires immediate discontinuation of the medication if toxicity is suspected [2]. Skin hyperpigmentation and bull's-eye maculopathy have also been reported, underscoring the need for regular dermatological and ophthalmological monitoring [3].
Conclusions
The use of hydroxychloroquine in the treatment of autoimmune diseases requires a careful balance between its therapeutic benefits and the potential risks of adverse effects. Regular ophthalmological monitoring is essential for early detection of retinopathy and prevention of irreversible vision loss. Additionally, it is crucial to remain vigilant for other adverse effects such as cardiomyopathy and skin hyperpigmentation. Adherence to dosing and monitoring guidelines, along with a multidisciplinary approach, can help minimize these risks and optimize patient management.
Referencias
- [1] SCREENING PRACTICES AND LATE DIAGNOSIS OF HYDROXYCHLOROQUINE RETINOPATHY IN ASIAN PATIENTS
- [2] Hydroxychloroquine-induced cardiomyopathy: case report, pathophysiology, diagnosis, and treatment
- [3] Hydroxychloroquine-induced hyperpigmentation of the skin and bull's-eye maculopathy in rheumatic patients: a case report and literature review
Created 6/1/2025
