Differentiating Crohn's Disease and Ulcerative Colitis: Endoscopic and Clinical Insights for Inflammatory Bowel Disease Management
Crohn's disease and ulcerative colitis are the two main forms of inflammatory bowel disease (IBD), and while they share some clinical features, their differentiation is crucial for the appropriate management of patients. Both conditions can present with chronic diarrhea, abdominal pain, and weight loss, but they differ in their endoscopic presentation and the distribution of inflammation throughout the gastrointestinal tract.
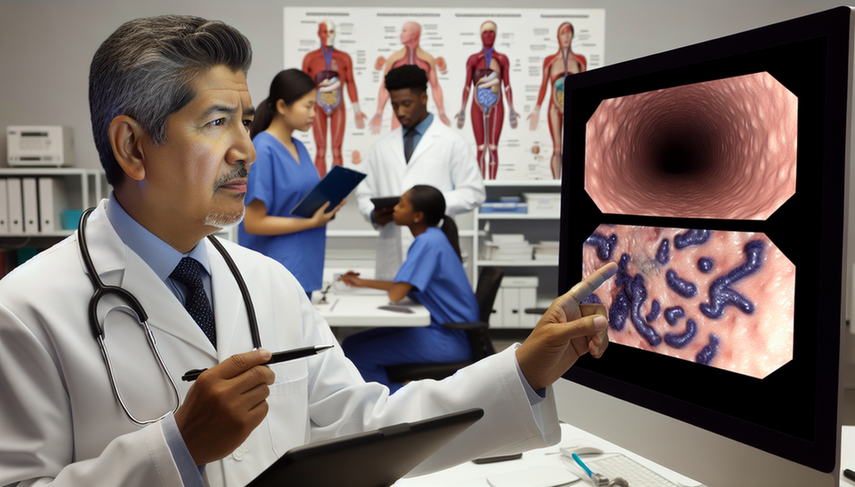
Endoscopic and Clinical Differentiation
Colonoscopy remains a fundamental tool for diagnosing IBD. In Crohn's disease, inflammation is typically transmural and can affect any part of the gastrointestinal tract, from the mouth to the anus, although it commonly involves the ileocecal region. Endoscopic features include discontinuous lesions, deep ulcers, and the characteristic cobblestone appearance. In contrast, ulcerative colitis is limited to the colon, with superficial inflammation primarily affecting the mucosa. The inflammation is continuous, starting at the rectum and extending retrogradely.
In addition to endoscopic differences, clinical manifestations can also aid in differentiation. Ulcerative colitis more frequently presents with rectal bleeding and bloody diarrhea, while Crohn's disease may exhibit a wider variety of symptoms, including fever, fatigue, and extraintestinal symptoms such as arthritis and uveitis.
Conclusions
Accurate differentiation between Crohn's disease and ulcerative colitis is essential for guiding treatment and improving patient outcomes. The combination of clinical, endoscopic, and histological findings is fundamental for precise diagnosis. Endosonography and non-invasive biomarkers such as fecal calprotectin are also emerging as useful tools for assessing disease activity and differentiating between these two conditions.
Referencias
- [1] Calprotectin in inflammatory bowel disease
- [2] Clinical presentation of Crohn's, ulcerative colitis, and indeterminate colitis: Symptoms, extraintestinal manifestations, and disease phenotypes
- [3] Diagnosis and classification of ulcerative colitis
- [4] Diagnosis and classification of Crohn's disease
- [5] Differentiation of Crohn's disease and ulcerative colitis using intestinal wall thickness of the colon: A Diagnostic accuracy study of endoscopic ultrasonography
Created 6/1/2025
